That bloating, fullness, or burning after eating? We’ve all been there. You brush it off as indigestion or “I ate too much,” because, in many cases, discomfort is something we tend to tolerate rather than address. Maybe you’ve had a heavy lunch at work, grabbed a quick snack between meetings, or even skipped meals to meet deadlines—things that feel like part of everyday life.
What is dyspepsia?
Dyspepsia refers to discomfort in the upper abdomen or chest. It can show up as bloating, nausea, a heavy feeling after eating, or that burning sensation we often call heartburn. While occasional discomfort is normal, if it keeps happening, it could be a sign that something needs attention. Dyspepsia often results from disrupted digestive processes like gastric motility disorders (where the stomach doesn’t empty properly) or acid reflux (when stomach acid irritates the oesophagus). Both conditions can cause discomfort, making dyspepsia more than just an occasional problem.
Why you shouldn’t ignore it
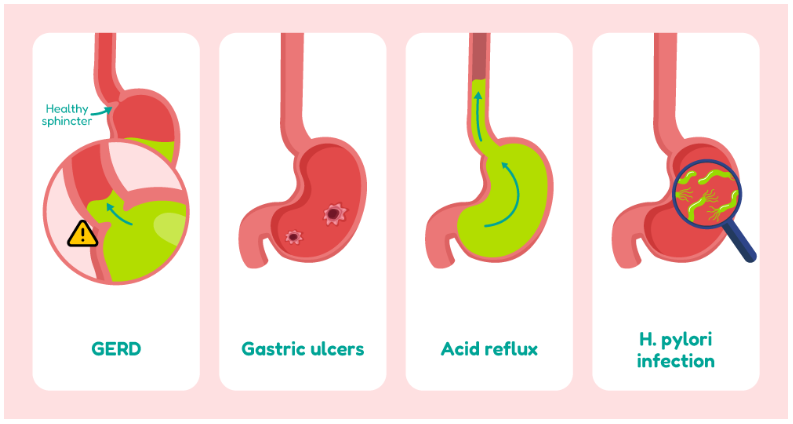
- Chronic discomfort: If you ignore dyspepsia, it may start to affect your focus, daily activities, and overall mood. Over time, untreated dyspepsia can lead to more serious complications like GERD and gastric ulcers.
- Potential long-term effects: Left untreated, conditions like acid reflux or H. pylori infection can cause further damage to your digestive system. Over time, this could lead to more invasive treatments or even surgery.
EXPERT INSIGHT
Dyspepsia is often dismissed or self-treated, but this can be risky, warns gastroenterologist Dr Lin. “People often overlook persistent indigestion symptoms, assuming they’re harmless. But symptoms like bloating, early fullness, nausea, and upper abdominal discomfort can be caused by a range of conditions, from gastro-oesophageal reflux disease (GERD) and peptic ulcers to gallbladder issues. In some cases, they could even point to non-digestive problems, such as an atypical presentation of coronary artery disease, which remains a leading cause of death in Singapore.
That’s why it’s important to seek medical attention if symptoms are frequent or ongoing, don’t improve with antacids, or if you find yourself needing antacids regularly.
Lifestyle adjustments for dyspepsia relief
Eat smaller, more frequent meals
Cut back on trigger foods
EXPERT TIP
In the Asia-Pacific region, certain dietary and lifestyle habits may contribute to dyspepsia, says Dr Lin. “Irregular eating patterns such as skipping breakfast or eating late at night, along with diets high in fatty, spicy, sugary, or highly processed foods are common contributors. Eating too quickly or having large meals can also put stress on the stomach and lead to discomfort.
Dr Lin adds that the temperature of food and drinks may also play a role. Cold drinks, for example, can trigger stronger stomach contractions and may worsen symptoms compared to warm ones. Simple lifestyle changes can make a meaningful difference, including eating slowly, having smaller and more frequent meals, and avoiding heavy meals close to bedtime.
Reducing intake of processed foods like instant noodles and packaged snacks, cutting down on alcohol, and limiting cold drinks can also help. Some people may benefit from temporarily avoiding dairy products, especially if they feel bloated after consuming them, since lactose intolerance tends to become more common with age.
Manage stress
EXPERT INSIGHT
Stress, anxiety, and other mental health issues play a significant role in triggering or worsening dyspepsia symptoms. There is a strong connection between the brain and the digestive system, and psychological factors like stress, anxiety, and depression are closely linked with how the body processes discomfort.
Studies have shown that people with dyspepsia often report higher levels of anxiety and depression compared to those with ulcers or individuals without digestive complaints. Interestingly, those whose symptoms improved over several months also experienced reduced levels of anxiety.
In a long-term Swedish study, individuals with anxiety at the outset were found to be more than seven times as likely to develop functional dyspepsia later on. This may be due to the way anxiety lowers pain tolerance and interferes with normal stomach function.
Exercise regularly
Lose excess weight
Wait before lying down after meals
Staying hydrated (but not during meals)
Elevate your head while sleeping
EXPERT INSIGHT
Differentiating between functional dyspepsia and symptoms caused by more serious gastrointestinal conditions often begins with a detailed history and physical examination. Clinicians consider not only the symptoms described by the patient, but also their age, medical history, family background, and any relevant risk factors.
In younger individuals without warning signs, initial testing may involve a non-invasive screen for Helicobacter pylori (H. pylori), a common bacterial infection linked to dyspepsia, ulcers, and an increased risk of stomach cancer. For patients with risk factors for heart disease, cardiac causes may also be considered.
If symptoms persist or the patient is older, typically over the age of 40, a gastroscopy may be recommended to directly examine the stomach and rule out more serious conditions.
How to explain your symptoms to your doctor
EXPERT INSIGHT
If dyspeptic symptoms continue despite initial treatment, further investigation is usually necessary. If the patient has not been tested for Helicobacter pylori (H. pylori), this is often the first step, using non-invasive methods such as a breath test or stool test.
If H. pylori has already been ruled out, or if the patient is over the age of 40, a gastroscopy is typically recommended. This procedure allows doctors to examine the stomach and upper digestive tract for signs of H. pylori, bile reflux, ulcers, or other potential causes.
When symptoms are thought to be related to acid or bile reflux but the gastroscopy is inconclusive, more specialised tests such as pH monitoring or impedance testing may be needed to clarify the diagnosis.